Thumb Basal Joint Arthritis


WHAT IS THUMB BASAL JOINT ARTHRITIS?
Thumb arthritis is common with aging and relates to the premature “wear and tear” of the cartilage forming the joint between the thumb and the wrist.
Pain is centered around this joint, and is made worse with forceful and repeated use of the hand. Thumb arthritis can cause severe pain, swelling, and decreased strength and range of motion, making it difficult to do simple tasks, such as turning doorknobs and opening jars.
This Condition occurs in women much more than it does in men, and often, although this premature degradation of the joint is usually present in both wrists, it is often MORE pronounced in the NON-DOMINANT hand !
Treatment generally involves a combination of medication and splints. Severe thumb arthritis might require surgery.
SYMPTOMS OF THUMB BASAL JOINT ARTHRITIS
Pain is the first and most common symptom of thumb arthritis. Pain can occur at the base of your thumb when you grip, grasp or pinch an object, or use your thumb to apply force.
Other signs and symptoms might include:
- Swelling, stiffness and tenderness at the base of your thumb
- Decreased strength when pinching or grasping objects
- Decreased range of motion
- Enlarged or bony appearance of the joint at the base of your thumb

IF YOU ARE SUFFERING FROM SYMPTOMS OF THUMB BASAL JOINT ARTHRITIS AND EVALUATING YOUR TREATMENT OPTIONS, SCHEDULE A CONSULTATION WITH DR. DANIEL DURAND TODAY.
WHAT CAUSES THUMB BASAL JOINT ARTHRITIS?
Thumb arthritis commonly occurs with aging. Previous trauma or injury to the thumb joint also can cause thumb arthritis.
In a normal thumb joint, cartilage covers the ends of the bones — acting as a cushion and allowing the bones to glide smoothly against each other. With thumb arthritis, the cartilage that covers the ends of the bones deteriorates, and its smooth surface roughens. The bones then rub against each other, resulting in friction and joint damage.
The damage to the joint might result in growth of new bone along the sides of the existing bone (bone spurs), which can produce noticeable lumps on your thumb joint.
Factors that can increase your risk of thumb arthritis include:
- Female sex.
- Age above 40 years.
- Obesity.
- Certain hereditary conditions, such as joint ligament laxity and malformed joints.
- Injuries to your thumb joint, such as fractures and sprains.
- Diseases that change the normal structure and function of cartilage, such as rheumatoid arthritis.
- Activities and jobs that put high stress on the thumb joint.

HOW IS THUMB ARTHRITIS DIAGNOSED?
A combination of physical examination and x-ray evaluation will enable the hand surgeon to tell how worn out the cartilage has become.
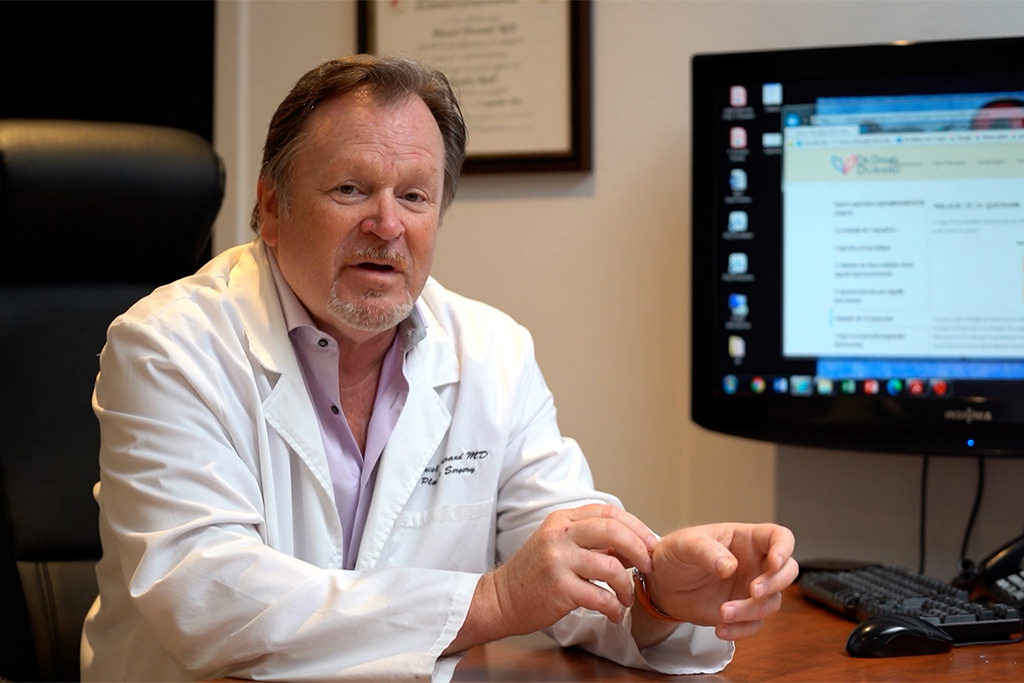
Dr. Durand will ask you about your symptoms, any prior injury, pain patterns, or activities that aggravate the condition.
- One of the tests used during the examination involves holding the joint firmly while moving the thumb. If pain or a gritty feeling results, or if a grinding sound (crepitus) can be heard, the bones are rubbing directly against each other.
- An x-ray may show deterioration of the joint as well as any bone spurs or calcium deposits that have developed.
Many people with arthritis at the base of the thumb also have symptoms of carpal tunnel syndrome, so Dr. Durand may check for that, as well.
WHEN SEEKING A DIAGNOSIS OR TREATMENT, IT’S BETTER TO SEE A DOCTOR SOONER RATHER THAN LATER. ONCE A CONDITION IS SEVERE, THE DISEASES ARE MORE DIFFICULT TO CORRECT.
EARLY INTERVENTION IS KEY TO AVOIDING PERMANENT DAMAGE. DEPENDING ON YOUR DIAGNOSIS, NONSURGICAL TREATMENT MAY BE AN OPTION.
HOW IS THUMB BASAL JOINT ARTHRITIS TREATED?
Depending on the severity of the condition, treatment can include a simple steroid injection into the area (in early cases), and in more severe presentations surgery may be required.
The end result is that patients after treatment are pain-free and are able to return to their usual daily activities in a comfortable manner. Dr. Durand will discuss the options with you and select the one that is best suited to your condition.
NON-SURGICAL TREATMENT
- A supportive splint to limit the movement of your thumb, and allow the joint to rest and heal. The splint may protect both the wrist and the thumb. It may be worn overnight or intermittently during the day.
- A steroid solution injection directly into the joint. This will usually provide relief for several months. However, these injections cannot be repeated indefinitely.
- Injections therapy. Injections therapy is a biological treatment designed to improve the biologic environment of the tissue. This involves obtaining a small sample of blood from the arm and centrifuging it (spinning it) to obtain platelets from the solution. Platelets are known for their high concentration of growth factors, which can be injected into the affected area.
SURGICAL TREATMENT
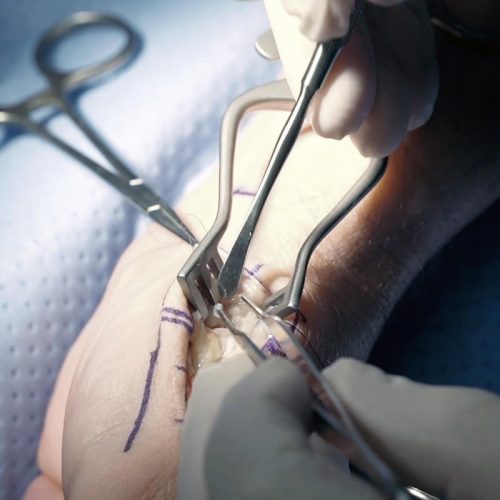
When nonsurgical treatment is no longer effective, surgery is an option. The operation can be performed on an outpatient basis, and several different procedures can be used.
- Joint fusion (arthrodesis). The bones in the affected joint are permanently fused. The fused joint can bear weight without pain, but has no flexibility.
- Osteotomy. The bones in the affected joint are repositioned to help correct deformities.
- Trapeziectomy. One of the bones in your thumb joint (trapezium) is removed.
- Joint replacement (arthroplasty). All or part of the affected joint is removed and replaced with a graft from one of your tendons.
These surgeries can all be done on an outpatient basis. After surgery, you can expect to wear a cast or splint over your thumb and wrist for up to six weeks. Once the cast is removed, you might have physical therapy to help you regain hand strength and movement.
HAND CARE WITH DR DANIEL DURAND
NOT ALL HAND AND WRIST CONDITIONS REQUIRE SURGICAL SOLUTIONS. OTHER TREATMENT OPTIONS ARE AVAILABLE FOR LESS SEVERE ISSUES. IF YOU’VE BEEN EXPERIENCING THUMB ARTHRITIS SYMPTOMS, SCHEDULE AN APPOINTMENT WITH DR. DANIEL DURAND TODAY!